Laparoscopy
Laparoscopy
Laparoscopy essentially means the visualization of the abdominal organs through a scope.
Laparoscope is a tubular instrument introduced into the abdomen through a 1cm opening near the umbilicus. A CCD camera is attached to the outer end of the laparoscope.
The uterus, ovary and the rest of the pelvic and abdominal organs can be visualized through the scope and viewed on a television monitor. Instruments passed through two tiny 5mm holes lower down in the abdomen can rectify any defects in the visualized organs.
Laparoscopy is usually done under General anaesthesia. The patient’s basic blood investigations are done and she is given a laxative the previous night. The patient has to be nil by mouth on the day of the procedure.
After the procedure she is kept in the recovery room for about 3-4 hours and then taken to her room.
Usually the patient is discharged on the next day.
The advent of laparoscopy has changed the practise of gynaecology quite a lot. Laparoscopy was started in India in the 80’s as a diagnostic tool. Gradually in the 90’s operative laparoscopy came into vogue and many surgical procedures which were done by opening the abdomen through a wound in the abdomen under direct vision could now be done through small holes in the abdomen with the help of the laparoscope. Laparoscopic surgery is also called key-hole surgery.
Role of laparoscopy in gynaecology
Laparoscopy is used to diagnose many conditions in gynaecology. Since operative laparoscopy is combined with diagnostic laparoscopy, the disease can quite often be cured at the same time as the diagnosis is made. Some of the conditions where laparoscopy as a diagnostic-cum operative tool is used are infertility, chronic pelvic pain, and endometriosis.
Infertility: When a couple fails to concieve after 6 months of unprotected intercourse, the couple could be said to be suffering from infertility or, inability to concieve. In some patients, after correction of other factors causing infertility have been corrected, the couple still fail to concieve, laparoscopy may be done to see if some other factors causing infertility are there . Some of the procedures done through the laparoscope in the infertile woman are:
Diagnosis of tubal block: If a woman fails to conceive inspite of medical treatment, it may be prudent to check and see if the fallopian tubes are patent. This can be achieved by injecting fluid into the uterus through a cannula introduced through the vagina. The fluid traverses the uterus , the fallopian tubes and then comes into the abdomen through the opening of the tubes called the fimbrial end. The fimbrial ends are visualized on the laparoscopy monitor . Any blocks near the fimbrial end or any adhesions near any part of the tube can be removed through laparoscopic instruments. If there is a block near the uterine end of the tube it can be rectified through another procedure called hysteroscopic cannulation which could be done at the same sitting.
Endometriosis: In some women, there may be severe abdominal cramps near the time of menstrual periods. This could be due to a disease called endometriosis. On examination of the vagina, the doctor may find some nodularities in the vagina. Endometriosis could cause infertility in many ways and the best way to correct it is through the laparoscope. Laparoscopic correction of endometriosis yields very high pregnancy rates.
Adhesive bands: Adhesions between the uterus and ovaries could cause infertility and these could be corrected through the laparoscope.
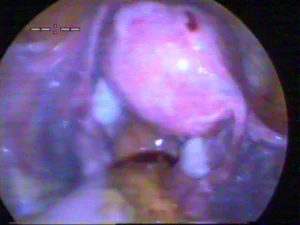
Correction of polycystic ovaries: In women who fail to ovulate because of a condition called polycystic ovarian syndrome, if oral medications fail to achieve ovulation, laparoscopic drilling of the ovaries may be done. In polycystic ovaries, the ovaries are fully of tiny follicles with fluid in it. A few of these fluid filled follicles are punctured using an instrument introduced through the laparoscope. This causes reduced levels of hormones called androgens and subsequently there is restoration of normal ovulation. A punctured ovary can be seen in the picture below.

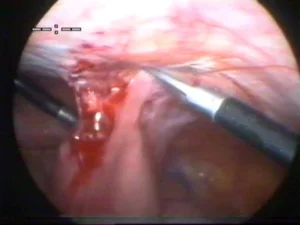
Continous low grade pain is a very common condition found in middleaged women. Quite often it is due to some low grade infection which can be cured when treated meticulously. In some cases of chronic pelvic pain(Defined as persistent pain of more than 6 months duration), laparoscopy may be useful in evaluating and curing the disease. How laparoscopy can be useful: 1. Sometimes pelvic infection leaves scars around the uterus and ovaries leading to pain. Release of painful adhesions through the laparoscope could give relief.The picture shows the ovary being stuck to the patient’s abdominal wall . This was causing severe abdominal pain. The cause could not be diagnosed either by examining the patient or by doing an ultrasonography. Diagnosis of the cause, along with release of adhesions cured the patient. 2. Severe pain during periods not cured with medicines could be treated by a procedure called uterosacral nerve vaporization. 3. In patients with a disease called endometriosis , laparoscopy helps in diagnosing the condition .Resection of endometriosis from all surfaces, specially the rectovaginal septal space could give relief. Endometriosis could cause severe pain during periods, pain during intercourse, crampy pain after passing stools, etc. |
|
4. Sometimes pelvic pain is due to dilated veins near the uterus. .In the picture, the blue colour seen in the picture is due to dilated veins. These veins extend to the side of the ovary and sometimes may go up to the upper abdomen. This is called pelvic venous congestion. Proper diagnosis can be made only from laparoscopy. The other definintive mode of diagnosis of this condition, viz;venography is not done for this condition routinely in India. After diagnosis proper medications could be given for cure. If not properly diagnosed, many a time the woman may be subjected to hysterectomy and this would not cure the disease and the woman would end up undergoing a major surgery without getting cure for her illness. |  |
5. Sometimes no abnormality is found on doing a laparoscopy and in these instances the patients are ready to accept the pain or control it with simple analgesics as they have the happy knowledge that nothing serious is wrong with them.
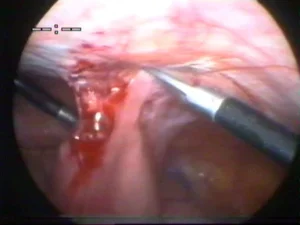
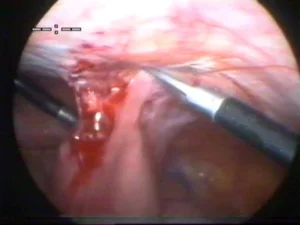
6. In some patients who have undergone major surgery like LSCS or hysterectomy the intestines may be adherent to the abdominal structures and may cause colicky pain when food passes through the adherent segment. The pain is severe a few hours after eating food . it decreases on its own in the initial phases, but persists when the condition becomes severe. In these cases, laparoscopic adhesiolysis may give relief from pain. Intestines attached to the abdomen can be seen in the picture in one such patient. Release of this intestine is being done using laparoscopic scissors. | 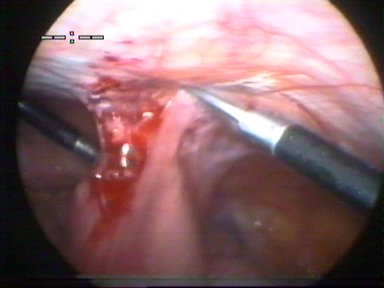 |
What it involves for the Patient:
Usually the patient is admitted the previous day, and an extensive bowel enema given . She is asked to be on oral fluids from the previous day. In case of minor adhesiolysis, she is allowed to go home the next day. But if extensive intestinal adhesions , the patient is observed for 4-5 days to make sure the intestines are working properly. Before surgery these patients are also warned about the possibility of intestinal injury which might lead to opening of the abdomen for bowel repair.
Laparoscopic surgeries in gynaecology |
Many of the surgeries done in the gynaecological patient are now done through laparoscopic guidance.
Advantages:
1. The cut or incision made on the abdomen being very small, there is less pain in the post-operative period.
2. Since the cut made in the layers of the abdomen is small, it causes less impairment to the strength of the abdominal wall. Thus the patient can start performing routine duties like lifting heavy weights much earlier.
3.Hospital stay is just for a couple of days or more, depending on the procedure, after laparoscopic surgery compared to open surgery.
4. The view offered through the laparoscope is very good and it is possible to do more meticulous surgery with the assistance of the laparoscope. Organs are seen as magnified images and thus minute changes in organs can be visualised and remedied with more accuracy.
Disadvantages:
1.Laparoscopic surgery involves a steep learning curve for the surgeon and not all gynaecologists can do good laparoscopic surgery. Thus the patient cannot know how much to expect from her gynaecologist.
2.Laparoscopic surgery involves the use of many electrical accessories like the light source, the camera, the cautery, etc and thus surgery could be delayed or interrupted when any of these equipments become defective.
3.Laparoscopy offers a two dimensional view instead of the three dimensional view offered by the open surgery. Thus in case of dire operative emergerncies, like the bleeding of a vessel, laparoscopic surgery may have to be converted to open surgery to do a quick job.
4.Not all centres offer laparoscopic surgery.
Use of laparoscopy in surgeries in gynaecology:
Many surgeries done in the past by open surgery are now done with the help of the laparoscope leading to earlier patient recovery. Some of them are listed below:
Tubal sterilisation:
Permenant sterilisation of the female can be done by applying silastic bands on the tubes. It takes just 10 minutes to perform. It can be done under local or general anaesthesia.
Ectopic pregnancy:
Sometimes, pregnancy, instead of lodging in the uterus gets lodged in the tubes or other places besides the uterus. If it grows there, it could endanger the life of the patient. Some of these pregnancies need surgical intervention, where the tubes are either removed along with the pregnancy (Salpingectomy) or cut to remove the pregnancy alone, leaving the tube behind(Salpingostomy). If the patient comes in severe shock, laparoscopy may not be possible. In all other patients, laparoscopic surgery is superior to laparotomy for the treatment of ectopic pregnancy.
Fibroid uterus:
Fibroids are non-cancerous growths in the uterus. They occur in many women without causing any symptoms. however, they cause symptoms in some patients and will need to be removed. This is called myomectomy and this can be done with the help of the laparoscope. However, the selection of cases which can be done laparoscopically depends on many factors, like the number of tumours, the size of fibroids, the experience of the laparoscopic surgeon and the equipment available in the hospital. Myomectomy causes a lot of bleeding during the surgery and the uterus needs to be stitched back after removing the fibroid. If suturing is not done properly after myomectomy, the uterus might burst at the time of childbearing and this could be disasterous. All this requies a lot of surgical skill and thus laparoscopic myomectomy is done only by experienced laparoscopic surgeons.Picture below shows laparoscopic myomectomy in progress. The white structure in the centre is the fibroid.

If there are many fibroids, specially deep seated one, it may not be possible to see all of them properly through the laparoscope and unless the surgeon is very sure of removing all of them laparoscopiclly, it is better to do open surgery for multiple fibroids.
Ovarian tumours:
The white structures beside the uterus, called ovaries may develop cystic or solid tumours in them. Cystic tumours contain fluid components and depending on the type of cyst it may be clear, amber cooured fluid or old blood in endometrioma. These cysts can be easily removed through the laparoscope. Any adhesions between the ovaries and the surrounding structures can be removed more meticulously through the view offered with the help of the laparoscope.
Removal of uterus/Hysterectomy:
The removal of uterus or hysterectomy is a common operation performed in the female nearing or following her menopause. This can be done with the help of the laparoscope with very little convalescence needed, compared to open surgery. Here, again, the selection of case suitable for laparoscopy depends on the skill of the surgeons. Less experienced surgeons may be unwilling to take up difficult cases, like patients with previous history of caesarian section or some other open surgery, or patients with very big tumours.
Conclusion:
Laparoscopy is the only diagnostic modality to diagnose some cases in gynaecology. As an operative tool it almost replacing open surgery and as more and more patients demand laparoscopy as the mode of surgery, there will be more training centres teaching laparoscopy with many more laparoscopic surgeons.
Laparoscopic Adesiolysis Chronic Pelvic Pain
Laparoscopic adhesiolyis is a surgery that can be done in only the best laparoscopy centres whether in kerala , thrissur, or elsewhere. Conditions like intestinal adhesions, ovarian adhesions, rectovaginal endometriosis, post operative adhesions, can all be treated with laparsocopic adhesiolyis.
Ovarian adhesions
Sometimes pelvic infection leaves scars around the uterus and ovaries leading to pain. Release of painful adhesions through the laparoscope could give relief. In the picture, the ovary is found stuck to the abdmominal wall. Every time the woman ovulates she could get severe pain due to such abnormal attachments. This could also give rise to painful menstrual periods. It may be difficult to detect this problem with any imaging modality except laparoscopy. Ultrasonography and CT scan may show no abnormality.

Endometriosis and rectovaginal endometriosis: In patients with a disease called endometriosis , laparoscopy helps in diagnosing the condition .Resection of endometriosis from all surfaces, specially the rectovaginal septal space could give relief.In the picture, the rectum is found adherent to the uterus and this adhesion is being released.
Pelvic venous congestion
Sometimes pelvic pain is due to dilated veins near the uterus. These veins extend to the side of the ovary andsometimes may go upto the upper abdomen.. This is called pelvic venous congestion. Patients get severe abdominal pain, menstrual pain, pain during intercourse,etc. Since they have many complaints, doctors sometimes also diagnose mental stress to be a cause of the problem. In the picture, the dilated blue veings can be seen by the side of the white ovaries and the long tubes.Proper diagnosis of pelvic venous congestion can be made only from laparoscopy. The other definintive mode of diagnosis of this condition,viz;venography is not done for this condition routinely in India. After diagnosis proper medications could be given for cure. If not properly diagnosed, many a time the woman may be subjected to hysterectomy and this would not cure the disease and the woman would end up undergoing a major surgery without getting cure for her illness.
Post operative adhesions:
In some patients who have undergone major surgery like LSCS or hysterectomy the intestines may be adherent to the abdominal structures and may cause colicky pain when food passes through the adherent segment. One such adhesion of intestine to the abdominal wall is seen in the picture. Laparoscopic release of these adhesions may give symptom relief. The author has done several cases of severe intestinal adhesions with good relief for the patients .
What laparoscopic adhesiolysis involves for the Patient:
Usually the patient is admitted the previous day, and an extensive bowel enema given . She is asked to be on oral fluids from the previous day. In case of minor adhesiolysis, she is allowed to go home the next day. But if extensive surgery has been done for intestinal adhesions , the patient is observed for 4-5 days to make sure the intestines are working properly. Before surgery these patients are also warned about the possibility of intestinal injury which might lead to opening of the abdomen for bowel repair.
Laparoscopic Ovarain Cystectomy

Laparoscopic ovarian cystectomy is a surgery where ovarian cysts are removed using an instrument called the laparoscope. Laparoscopic surgery for ovarian cysts give the following advantages;
- Faster recovery, after the procedure, as the patient can go home faster.
- More meticulous surgery, as magnification offered by the laparoscope makes the organs clearer to the surgeon.
- Very few scars on the abdomen, so the stigma of having undergone surgery is less, specially for unmarried girls.
Indications
- Benign ovarian cysts. These are noncancerous tumours of the ovary, which are harmless at present, as diagnosed by ultrasonography and other investigative modalities. Usually, if the cyst diagnosed on ultrasonography does not disappear in 3 months and the size is more than 6cm, a benign ovarian cyst is diagnosed.
- Twisted ovarian cyst. Some cysts are not tumours, but they make the ovary undergo torsion and multiple twists will jeopardise the blood supply of the ovary. This causes severe abdominal pain and sometimes vomiting. This necessitates immediate surgery to untwist the ovarian cyst and do a cystectomy.
- Definite tumours diagnosed, like endometrioma, dermoid etc.
Ovarian cystectomy under Dr.Shobhana: What can be expected:
Preoperative:
- The patient has to undergo many blood tests , X-ray chest,and ECG to make sure she is medically fit.
- In case of twisted ovarian cysts, surgery has to be done on an emergency basis. In all other cases, the protocol below will be followed.
- If there are any deficiencies, like high blood sugar, high blood pressure, or changes in ECG, then these deficiencies have to be corrected.
- On the day prior to surgery, She has to take only oral fluids after 4PM. She will be given 2 litres of a special fluid , which will make her empty her bowel completely. This is to ensure that the bowels do not come too much near the area of surgery near the uterus.
- She should not take food or any fluids after 10PM the previous day.
- She will be admitted in the morning of surgery and surgery will be done in the afternoon.
- She will be given enough fluids intravenously in the morning so that she does not feel hungry or thirsty.
Operative time.
For compartively simple ovarian cysts, operative time can be expected to be half an hour to one hour. But in complicated cases like patients with previous surgery, severe adhesions, or advanced endometriosis,surgery can be prolonged.
Post operative period:
After surgery, the patient will be shown to the relatives and wheeled back to the post operative care room where she will be observed for complications for about 2 hours. After that she will be taken to the room.
Following surgery, women may feel nauseous as a side effect of the general anaesthetic and experience some abdominal pain and discomfort. These are relieved with medications.There may also be some vaginal bleeding which should reduce after a few days. Women are encouraged to get up and walk around on the first day following surgery to avoid constipation and gaseous bloating of abdomen and decrease the risk of blood clots and lung infections
She can start oral sips 6 hours after surgery.She can start food next day morning. Since the patient is well hydrated and enough glucose has gone into her system, she may not feel hungry or thirsty and bystanders should not force her to eat or drink, because they feel scared.
If she is very fit, she can be discharged next day. Usually, patients take 1 or 2 days to recuperate from surgery.
Some patients, requiring difficult surgery , with bowel adhesions, will take longer to recuperate. This is because, the bowel takes longer to get back to normal.
How much rest is need after Cystectomy: She can start small tasks after she is discharged. She can travel by bus, bend, climb stairs, lift objects from the kitchen platform to the cooking gas, and so on. She can start work within a week.
For a video on ovarian cystectomy for endometrioma by Dr.Shobhana Mohandas, click on:
- Video on gangrenous ovarian cyst: http://keralagynaecology.com/video/gangrenous-ovarian-cyst/
Ovarian cyst in this patient had undergone gangrene in this patient because of delay in treatment. But fortunately becuase of the minimal amout of ovary that could be left behind in the patient, she could undergo two spontaneous pregnancies a few years after her marriage.
Laparoscopic Myomectomy

Laparoscopic myomectomy is a fertility-sparing procedure to remove fibroids, which are non-cancerous tumors that affect up to 80 percent of women by age 50. The uterus is left intact after the procedure. Removing them laparoscopically lets the patient recover faster after the procedure. She will have just 2 or 3 small incisions on her abdomen and she can get back to work faster.
Once a patient is through recovery from a myomectomy, menstrual cycles should normalize, and there should be a noticeable difference in the level of pain. After at least 3 months, women can pursue fertility options. It is essential for the uterus to be completely healed before trying to conceive.
If hysterectomy for fibroids is indicated, it is important to get a second opinion. Age and fertility are the most important factors for these procedures. For some patients, laparoscopic myomectomy may still be an option. The author has removed fibroids as large as 10 cm laparoscopically and the patients have delivered at term after laparoscopic myomectomy. Even 6-7 fibroids have been removed laparoscopically by Dr.Shobhana Mohandas on request by the patient. It is not recommended for women who are past fertility to undergo a myomectomy, as it is a more invasive procedure than a hysterectomy. However, some patients demand that hysterectomy should not be done for them and in those cases, and in younger patients, even after completing their family, laparoscopic myomectomy is a choice.
Dr.Shobhana Mohandas has been practicing laparoscopic surgery for more than 2000 patients at a high level of expertise and several patients have undergone this procedure under her care.
Advantages of laparoscopic procedure;
Laparoscopic myomectomy offers many advantages compared to open abdominal surgery such as:
- Enhanced recovery
- Short hospital stay.
- Cosmetically improved scar.
- Reduced adhesions (scarring) from the procedure.
- Comparable pregnancy rates.
Length of procedure
For average size fibroids, myomectomy by Dr.Shobhana takes just over an hour. Large fibroids and multiple fibroids may take longer.
The less time under anesthesia is better for the patient, but it is important to also perform a thorough procedure.
Hospital stay:
Generally the procedure is done in the afternoon and the patient goes home next day itself. In case there are accompanying pathologies like adhesions due to endometriosis, convalescence may be longer.
How long is the Laparoscopic myomectomy recovery?
Fibroid removal with Laparoscopy performed using just 3-4 small incisions, so the pain from surgery is significantly less Most women are back to their normal activities within 10-14 days.
Pregnancy or childbirth complications. A myomectomy can increase certain risks during delivery if you become pregnant. If there are deep incisions in your uterine wall, there may be need for cesarean section in a subsequent pregnancy to avoid rupture of uterus during labour, a very rare complication of pregnancy. Under Dr.Shobhana’s care, post myomectomy patients have undergone normal delivery or cesarian section depending on site and size of the tumour.
After effects:
After surgery to remove one or more fibroids, you may feel some pain in your belly for several days. Your belly may also be swollen. You may have a change in your bowel movements for a few days. And you may have some cramping for the first week. You will feel tired, but will be able to eat and drink normally, walk around and go to the toilet.
Shoulder or back pain usually caused by the gas after laparoscopy in other centres is almost not seen under care of Dr.Shobhana as the gas is sucked before closing the abdomen.To help with pain, medicines will be prescribed.. You will need 2 or more weeks to fully recover.
You may have light bleeding for up to 8 weeks. You may have a brown or reddish brown vaginal discharge or spotting for a few weeks or until your first period. This is normal. Expect your first two periods to start early or late. They may be more painful or heavy than usual.
How are adhesions prevented?
With laparoscopic approach, there is minimal tissue handling which reduces risk of adhesions. Saline irrigation is also constantly in use which prevents drying of tissues and blood clots from sticking to the tissues. Meticulous control of bleeding also is essential.
Laparoscopic Hysterectomy
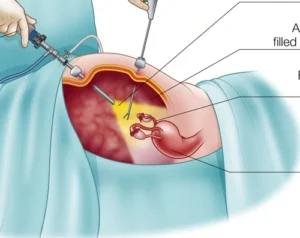
Laparoscopic hysterectomy essentially means removal of the uterus using the help of the instrument, Laparoscope. Laparoscopy essentially means the visualization of the abdominal organs through a scope. Laparoscope is a tubular instrument introduced into the abdomen through a 1cm opening near the umbilicus. A CCD camera is attached to the outer end of the laparoscope.
The uterus, ovary and the rest of the pelvic and abdominal organs can be visualized through the scope and viewed on a television monitor. Instruments passed through two tiny 5mm holes lower down in the abdomen can rectify any defects in the visualized organs . In laparoscopic hysterectomy, connections of the uterus to the body are cut with instruments using the laparoscope. The uterus is then removed vaginally.
Advantages for the patient: There being very few stitches on the abdomen, the procedure is fairly painless. Laparoscopy gives an enlarged view of the internal organs to the doctor and minute corrections can be made in a better fashion.

How patients are admitted under Dr.Shobhana for laparoscopic hysterectomy.
Preoperative:
- The patient has to undergo many blood tests , X-ray chest,and ECG to make sure she is medically fit.
- If there are any deficiencies, like high blood sugar, high blood pressure, or changes in ECG, then these deficiencies have to be corrected.
- On the day prior to surgery, She has to take only oral fluids after 4PM. She will be given 2 litres of a special fluid , which will make her empty her bowel completely. This is to ensure that the bowels do not come too much near the area of surgery near the uterus.
- She should not take food or any fluids after 10PM the previous day.
- She will be admitted in the morning of surgery and surgery will be done in the afternoon.
- She will be given enough fluids intravenously in the morning so that she does not feel hungry or thirsty.
- 2 bottles of blood have to be arranged, one bottle ready at site.
Operative time.
For compartively small uterus, operative time can be expected to be one hour. But in complicated cases like patients with previous surgery, severe adhesions, or large uterus, surgery can be prolonged.
Post operative period:
After surgery, the patient will be shown to the relatives and wheeled back to the post operative care room where she will be observed for complications for about 2 hours. After that she will be taken to the room.
Following surgery, women may feel nauseous as a side effect of the general anaesthetic and experience some abdominal pain and discomfort. These are relieved with medications.There may also be some vaginal bleeding which should reduce after a few days. Women are encouraged to get up and walk around on the first day following surgery to avoid constipation and gaseous bloating of abdomen and decrease the risk of blood clots and lung infections
She can start oral sips 6 hours after surgery.She can start food next day morning. Since the patient is well hydrated and enough glucose has gone into her system, she may not feel hungry or thirsty and bystanders should not force her to eat or drink, because they feel scared.
If she is very fit, she can be discharged next day. Usually, patients take 1 or 2 days to recuperate from surgery. After taking food some patients may feel some bloating sensation in the abdomen due to gaseous distension in the evening. This is usually relieved with medicines. After the bowel starts working like before, the patient will pass flatus. After this, she will begin to feel much better.
She can be discharged the 3rd day, usually if she feels fit and fine. Some patients, requiring difficult surgery , with bowel adhesions, will take longer to recuperate. This is because, the bowel takes longer to get back to normal.
Hospital stay:
How much rest is need after hysterectomy: She can start small tasks after she is discharged. She can travel by bus, bend, climb stairs, lift objects from the kitchen platform to the cooking gas, and so on. She should avoid sudden moments like jumping or gardening for 1 month. This is important, because lack of pain may lead to the patient forgetting that she is post operative and she may indulge in strenuous activities. Dull aching pain and feeling tired can be expected, for a few days. This is because healing processes are taking place inside the body. As long as these symptoms reduce day by day, it is okay. If it is increasing one has to visit the doctor. Light blood stained discharge can be expected for 6 weeks after surgery. This will settle. This is due to healing of the vaginal wound. Frank bleeding has to be reported and a visit to the doctor made.
Putting on weight after hysterectomy
Studies have shown that there is a slightly higher risk for weight gain in the first year after surgery, but this is more common in women who were already heavier at the time of surgery.It may not be entirely an after effect of surgery. Being housebound and decreasing the level of activities during recuperation can also lead to weight gain. Proper diet and exercise can prevent this weight gain. In women who have had their ovaries removed, androgenic hormones can start acting leading to weight gain. Bulging of the abdomen due to weak abdominal muscles can happen after open surgery, but is less likely after vaginal hysterectomy or laparoscopic hysterectomy.
Back pain after hysterectomy?
If hysterectomy is done by opening the abdomen, women may hunch over to protect their abdomen and if they do this for long enough do develop back pain because they have changed their centre of gravity. It is therefore important to walk up-right as soon as you are able to. This is unlikely after vaginal or laparoscopic hysterectomy. It is common for women in their middle age to get lumbosacral strain . This may happen with or without hysterectomy. However, if a woman has undergone hysterectomy, she may attribute it to hysterectomy.
Can I have sex after hysterectomy?
You will be advised not to have sex for around four to six weeks after having a hysterectomy. This should allow time for scars to heal and any vaginal discharge or bleeding to stop. Having the uterus removed can cause women to worry about feeling less womanly, or losing their sexual attractiveness. However, these feelings don’t last long. Interest in sex may return as recovery progresses.
What are the complications of hysterectomy?
- Serious but uncommon complications include:
- Bleeding
- Damage to nearby organs like bladder, urethra .
- Pelvic infection.
- Repeat surgery for bleeding or wound problems.
- Clot formation in the leg veins.
- Rarely damage to bowel also can happen.
The other frequent minor side effects include wound infection, urinary infection and abnormal sensations around the wound area.